Overview

Flat feet are a usually painless condition where the arches on the inside of your feet are completely collapsed arches so that the entire sole of your feet touch the floor when standing. Flat feet can develop after an injury to the foot, such as a ligament, tendon or muscle tear, or as a result of arthritis or they may develop because the condition runs in the family. People with flat feet often complain of their feet rolling inwards when walking or a feeling of their foot collapsing.
Causes
Fallen arches have many causes. If you have fallen arches, or flat feet, the normal arch in the middle of your foot is not curved properly. You can have this condition called ples planus in medical terms and never have any symptoms. However, fallen arches can lead to foot pain, fatigue or more serious conditions. If fallen arches alter the way you walk, you may eventually develop knee, hip and low back pain. Your foot may lose normal range of motion making it hard to rise up onto your toes. In some cases, your feet can become swollen. If you have this condition, talk to your doctor about an appropriate treatment plan.
Symptoms
Symptoms that should be checked by a pediatrician include foot pain, sores or pressure areas on the inner side of the foot, a stiff foot, limited side-to-side foot motion, or limited up-and-down ankle motion. For further treatment you should see a pediatric orthopedic surgeon or podiatrist experienced in childhood foot conditions.
Diagnosis
You can test yourself to see if you have flat feet or fallen arches by using a simple home experiment. First, dip your feet in water. Then step on a hard flat surface, like a dry floor or a piece of paper on the floor, where your footprints will show. Step away and examine your foot prints. If you see complete/full imprints of your feet on the floor, you may have fallen arches. However, it?s important to seek a second option from a podiatrist if you suspect you have fallen arches so they can properly diagnose and treat you.
What causes pes planus?
Non Surgical Treatment
Normally, flat feet disappear by age six as the feet become less flexible and the arches develop. Only about 1 or 2 out of every 10 children will continue to have flat feet into adulthood. For children who do not develop an arch, treatment is not recommended unless the foot is stiff or painful. Shoe inserts won?t help your child develop an arch, and may cause more problems than the flat feet themselves. However, certain forms of flat feet may need to be treated differently. For instance, a child may have tightness of the heel cord (Achilles tendon) that limits the motion of his foot. This tightness can result in a flat foot, but it usually can be treated with special stretching exercises to lengthen the heel cord. Rarely, a child will have truly rigid flat feet, a condition that can cause problems.
Surgical Treatment

This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer). Flat feet and fallen arches are common conditions that are in most cases asymptomatic. However, in patients who do have symptoms, treatments are available that can help reduce pain and promote efficient movement. Orthotic devices are well recognised as an excellent treatment and podiatrists can offer these different treatment modalities as individualised treatments for patients.
Prevention
It?s time to take a long hard look at what?s in your closet. Now is the time to toss out shoes that are well worn. You also need to say good-bye to thin-soled shoes that offer zero arch support. If you?re overweight, fallen arches may be a sign the universe is trying to tell you something. You need to lose weight, and odds are, fallen arches are but one of many physical discomforts you are experiencing.

Flat feet are a usually painless condition where the arches on the inside of your feet are completely collapsed arches so that the entire sole of your feet touch the floor when standing. Flat feet can develop after an injury to the foot, such as a ligament, tendon or muscle tear, or as a result of arthritis or they may develop because the condition runs in the family. People with flat feet often complain of their feet rolling inwards when walking or a feeling of their foot collapsing.
Causes
Fallen arches have many causes. If you have fallen arches, or flat feet, the normal arch in the middle of your foot is not curved properly. You can have this condition called ples planus in medical terms and never have any symptoms. However, fallen arches can lead to foot pain, fatigue or more serious conditions. If fallen arches alter the way you walk, you may eventually develop knee, hip and low back pain. Your foot may lose normal range of motion making it hard to rise up onto your toes. In some cases, your feet can become swollen. If you have this condition, talk to your doctor about an appropriate treatment plan.
Symptoms
Symptoms that should be checked by a pediatrician include foot pain, sores or pressure areas on the inner side of the foot, a stiff foot, limited side-to-side foot motion, or limited up-and-down ankle motion. For further treatment you should see a pediatric orthopedic surgeon or podiatrist experienced in childhood foot conditions.
Diagnosis
You can test yourself to see if you have flat feet or fallen arches by using a simple home experiment. First, dip your feet in water. Then step on a hard flat surface, like a dry floor or a piece of paper on the floor, where your footprints will show. Step away and examine your foot prints. If you see complete/full imprints of your feet on the floor, you may have fallen arches. However, it?s important to seek a second option from a podiatrist if you suspect you have fallen arches so they can properly diagnose and treat you.
What causes pes planus?
Non Surgical Treatment
Normally, flat feet disappear by age six as the feet become less flexible and the arches develop. Only about 1 or 2 out of every 10 children will continue to have flat feet into adulthood. For children who do not develop an arch, treatment is not recommended unless the foot is stiff or painful. Shoe inserts won?t help your child develop an arch, and may cause more problems than the flat feet themselves. However, certain forms of flat feet may need to be treated differently. For instance, a child may have tightness of the heel cord (Achilles tendon) that limits the motion of his foot. This tightness can result in a flat foot, but it usually can be treated with special stretching exercises to lengthen the heel cord. Rarely, a child will have truly rigid flat feet, a condition that can cause problems.
Surgical Treatment

This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer). Flat feet and fallen arches are common conditions that are in most cases asymptomatic. However, in patients who do have symptoms, treatments are available that can help reduce pain and promote efficient movement. Orthotic devices are well recognised as an excellent treatment and podiatrists can offer these different treatment modalities as individualised treatments for patients.
Prevention
It?s time to take a long hard look at what?s in your closet. Now is the time to toss out shoes that are well worn. You also need to say good-bye to thin-soled shoes that offer zero arch support. If you?re overweight, fallen arches may be a sign the universe is trying to tell you something. You need to lose weight, and odds are, fallen arches are but one of many physical discomforts you are experiencing.








 Overview
Overview Symptoms
Symptoms Prevention
Prevention A bunion (hallux valgus) is a deformity of the base joint of the big toe. The cause is not clear in many cases. The deformity may cause the foot to rub on shoes, which may cause inflammation and pain. Good footwear is often all that is needed to ease symptoms. An operation to correct the deformity is an option if good footwear does not ease symptoms.
A bunion (hallux valgus) is a deformity of the base joint of the big toe. The cause is not clear in many cases. The deformity may cause the foot to rub on shoes, which may cause inflammation and pain. Good footwear is often all that is needed to ease symptoms. An operation to correct the deformity is an option if good footwear does not ease symptoms.
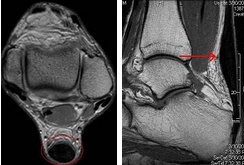
 When a tendon ruptures it can be extremely painful and cause a disability of the foot that then subsequently causes damage to the ankle joints. The tendons in the ankle include: the peroneals (peroneus brevis, peroneus longus,) anterior tibialis, posterior tibialis, and Achilles tendon. Any of these structures can become ruptured, which is a serious condition that will typically require surgery to fix.
When a tendon ruptures it can be extremely painful and cause a disability of the foot that then subsequently causes damage to the ankle joints. The tendons in the ankle include: the peroneals (peroneus brevis, peroneus longus,) anterior tibialis, posterior tibialis, and Achilles tendon. Any of these structures can become ruptured, which is a serious condition that will typically require surgery to fix.